Diabetic Macular Edema in Baltimore
Also serving Pikesville, Catonsville, Glen Burnie, & Rosedale
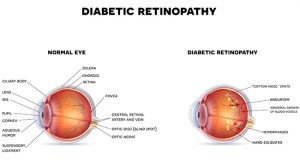 One of the most common causes of visual impairment and blindness in people with diabetes is a complication of diabetic retinopathy called diabetic macular edema (DME). Diabetic macular edema results in swelling in the macula, the portion of the retina responsible for clear central vision. The effects of DME can include blurry vision, image distortion, color or contrast changes, floaters or dark spots in the field of vision.
One of the most common causes of visual impairment and blindness in people with diabetes is a complication of diabetic retinopathy called diabetic macular edema (DME). Diabetic macular edema results in swelling in the macula, the portion of the retina responsible for clear central vision. The effects of DME can include blurry vision, image distortion, color or contrast changes, floaters or dark spots in the field of vision.
The visual impairments of DME can affect day-to-day life in a variety of ways. They can make it difficult to see and take the proper medications, drive, stay active or even work. Undetected DME will gradually worsen and vision will continue to deteriorate. If untreated, DME can result in permanent vision loss and even legal blindness.
To ensure quality of vision and of life, people diagnosed with diabetic macular edema should seek the expertise of retinal specialists like Dr. Michael Elman and Dr. Sidney Schechet, who can suggest the most appropriate treatment.
What Causes Diabetic Macular Edema?
Consistently high blood sugar levels can damage the tiny blood vessels in the retina, which is the layer of light-sensitive tissue at the back of the eye. These damaged blood vessels leak blood and fluid into the retina, causing swelling of the retina. Left untreated, the fluid can build up and cause the macula, or the central part of the retina responsible for sharp straight-ahead vision, to thicken and swell. This impairs the macula’s ability to function properly, and as a result, central vision suffers.
According to the National Eye Institute, which is a part of the National Institutes of Health, approximately 10 percent of the 7.7 million Americans with diabetes have diabetic macular edema. It is the leading cause of vision loss from diabetes today.
Detection and Diagnosis
Diabetic macular edema usually causes objects in the center of the field of vision to appear blurry or wavy. Colors may appear faded or dull.
Individuals who experience similar symptoms should see our retinal specialists for a complete eye exam and testing. Once they confirm DME and identify the severity of the condition, our doctors can outline the possible treatment solutions and recommend the most appropriate treatment or combination of treatments.
Treating Diabetic Macular Edema
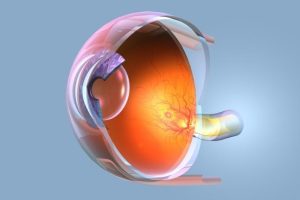
In the past, retinal specialists recommended laser therapy to patients with DME to seal off leaking blood vessels in the retina. Nowadays, the greatest success comes from painlessly injecting anti-VEGF medications directly into the eye.
Anti-VEGF medications block a protein called vascular endothelial growth factor (VEGF) that causes normal blood vessels to leak and stimulates the growth of abnormal blood vessels. In a healthy eye, VEGF does not adversely affect blood vessel growth. However, with conditions like diabetic retinopathy, VEGF can become overactive and cause the retinal blood vessels to leak. Injecting anti-VEGF medications into the eye has been shown to reverse the progression of diabetic macular edema. A series of injections over time is normally recommended. The eyes are numbed prior to the injections to prevent any discomfort.
Successfully managing DME requires keeping diabetes itself under control. People with DME are encouraged to take diabetes medications as prescribed, eat a healthy diet, exercise routinely and see their doctors regularly for follow-up. Control of high blood pressure is also very important to limit the leakage from diabetic macular edema.
Preventing Macular Edema
 There is no proven way to avoid macular edema. However, maintaining a healthy lifestyle with a balanced diet and regular exercise offers the best chances at reducing the risk of DME. People with diabetes should see an eye doctor annually for comprehensive dilated eye exams.
There is no proven way to avoid macular edema. However, maintaining a healthy lifestyle with a balanced diet and regular exercise offers the best chances at reducing the risk of DME. People with diabetes should see an eye doctor annually for comprehensive dilated eye exams.
Contact Elman Retina Group
If you have been diagnosed with diabetic macular edema, or you have noticed visual symptoms consistent with the disease, our doctors can help. Please call or email the Elman Retina Group today to request a consultation with our trusted retinal specialists.
Macular Edema FAQs
Will Macular Edema Go Away Without Treatment?
 In rare instances, macular edema may go away on its own, but this is highly unlikely and depends on the cause. When the macula is swollen, it can’t function properly, which leads to mild to severe central vision loss. Macular edema is often a complication in people with diabetes who have diabetic retinopathy, which damages the tiny blood vessels in the eye and leads to vision loss. Previous eye surgery, such as cataract surgery, can increase your risk of macular edema because of the irritation to blood vessels and the potential for leaking. Other possible causes include age-related macular degeneration, uveitis, retinal vein occlusion and vein blockages in the retina. In these instances, macular edema is unlikely to go away without treatment.
In rare instances, macular edema may go away on its own, but this is highly unlikely and depends on the cause. When the macula is swollen, it can’t function properly, which leads to mild to severe central vision loss. Macular edema is often a complication in people with diabetes who have diabetic retinopathy, which damages the tiny blood vessels in the eye and leads to vision loss. Previous eye surgery, such as cataract surgery, can increase your risk of macular edema because of the irritation to blood vessels and the potential for leaking. Other possible causes include age-related macular degeneration, uveitis, retinal vein occlusion and vein blockages in the retina. In these instances, macular edema is unlikely to go away without treatment.
What are Common Macular Edema Symptoms?
The fluid buildup in the macula caused by abnormal leakage from damaged blood vessels affects your ability to see directly in front of you. The swelling and thickening of the macula typically cause blurred vision, distorted vision and muted colors in the center of your eyesight. People may experience mild vision impairment or noticeable vision loss with macular edema. Some patients don’t notice the vision disturbances until the damage is advanced, especially if it only affects one eye.
How Long Does Macular Edema Last?
Macular edema can be effectively treated, but there is no cure. If you do not treat the condition, you run the risk of vision loss and legal blindness due to the loss of central vision. The standard of care for many causes of macular edema is Anti-VEGF injections such as for diabetic macular edema and cystoid macular edema from retinal vein occlusion. Other treatment options include anti-inflammatory treatments such as corticosteroids (from steroid drops to intraocular injections). Nonsteroidal anti-inflammatory eye drops used before and after cataract surgery may lower your risk of macular edema. Typically, as a last resort, the vitrectomy surgery may improve chronic and refractory macular edema.
Can Stress Cause Fluid Behind the Eyes?
Researchers have linked macular edema, specifically sub-retinal fluid, to mental stress and persons who lead hectic lives, though it’s unclear if stress is a cause or a consequence. Stress affects many aspects of your overall health, and your eyesight is no exception. Chronic stress disrupts the digestive system and impacts blood circulation. Your stress levels may limit the nutrients delivered to your eyes, in turn putting you at risk for development of macular edema and other eye diseases. The hormone cortisol is released during times of mental stress and is linked to inflammation and leakage in the eye, leading to fluid buildup in the back of the eye.
Can You Go Blind from Macular Edema?
While macular edema isn’t an emergency that can cause instant blindness, it can lead to irreversible vision loss if left untreated over prolonged periods of time, so timely diagnosis and treatment are essential. Our eye doctors will figure out the underlying cause of and discuss your macular edema treatment options during your comprehensive dilated eye exam.
How Can I Lower My Chances for Macular Edema?
Sometimes, you can’t prevent macular edema, such as when it’s caused by previous eye surgery or linked with an eye disease such as age-related macular degeneration. You can lower your chances of developing macular edema by eating a nutritious, well-balanced diet, reducing your stress levels, and managing health conditions such as diabetes, hypertension and inflammatory diseases.



