Understanding the Stages of Diabetic Retinopathy
Submitted by Elman Retina Group on September 15, 2020
Elevated blood sugar, blood pressure and cholesterol levels and increased body weight are associated with uncontrolled diabetes and can damage the delicate blood vessels of the retina, causing a disease called diabetic retinopathy. In the early stages of diabetic retinopathy, vision loss may be prevented or limited; but as the condition advances, it becomes more difficult to prevent vision loss.
Read on as the retinal specialists at Elman Retina Group shed light on the stages of diabetic retinopathy.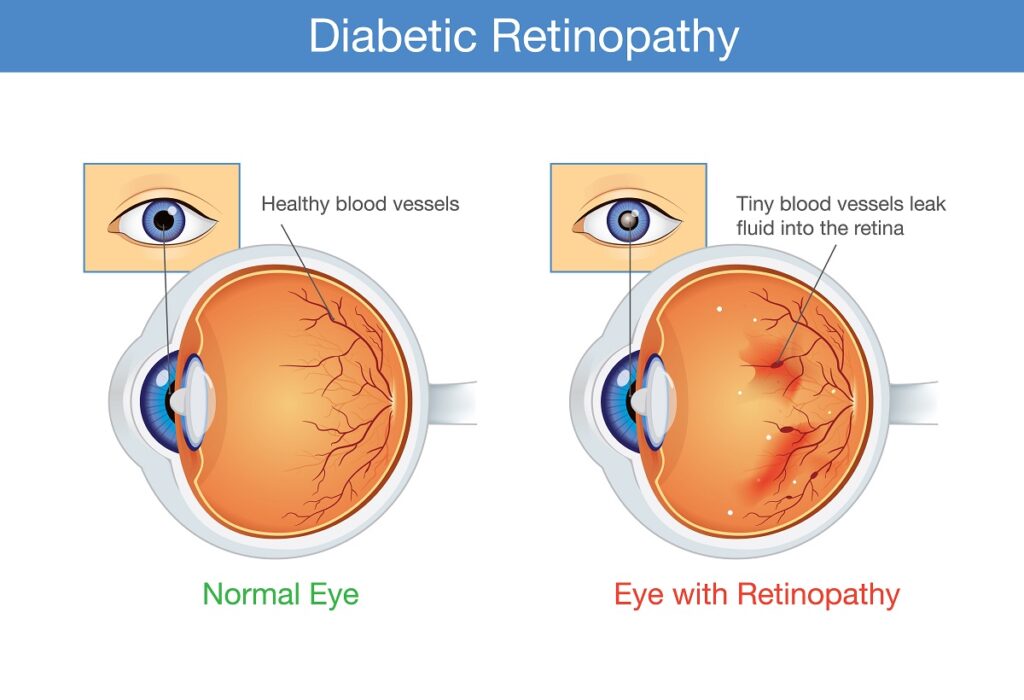
Non-Proliferative Retinopathy
Non-proliferative diabetic retinopathy is the earlier and less serious stage of the disease. Due to damage from elevated blood sugar levels, the tiny blood vessels of the retina start to swell and leak fluid and blood. The leaking causes swelling inside the retina called macular edema, which is a common cause of visual impairment in people with diabetes.
As non-proliferative retinopathy advances, the blood vessels may become blocked or closed off, and new abnormal blood vessels may start to grow and form in the wrong parts of the retina. Vision is usually unaffected in the non-proliferative stages, but it is best for the retina doctor to watch these changes closely every few months to ensure it doesn’t worsen to the “proliferative” stage.
Proliferative Diabetic Retinopathy
The more serious form of the disease, proliferative diabetic retinopathy is characterized by a process known as neovascularization. When the blood vessels of the retina become blocked, the retina is deprived of the oxygen and nutrients it needs to thrive. Sensing its limited blood supply, the retina responds by growing new abnormal blood vessels in the wrong parts of the retina. But the new blood vessels are abnormal and do not provide proper blood flow. They are extremely fragile and, as they grow, can leak blood into the vitreous. Sometimes this bleeding causes visual distortions called floaters; if the bleeding is severe enough, it can partially or completely impair vision.
In some cases, the formation of the new, abnormal blood vessels leads to the development of scar tissue, or fibrosis, in the retina. Scar tissue may cause the retina to wrinkle or “pucker,” or even detach from its normal position along the back of the eye, which is referred to as “tractional retinal detachment.” Depending on the complication, central vision loss can occur.
Another complication to watch out for is the growth of these abnormal blood vessels blocking the drainage angle, the natural mechanism by which fluid exits the eye. If this occurs, pressure inside the eye can spike very quickly, causing neovascular angle-closure glaucoma.
Early Detection Is Key
With a better understanding of the stages of diabetic retinopathy, you can see how important it is to catch the disease quickly. At Elman Retina Group, our experienced doctors are focused on slowing the progression of the disease and restoring vision however possible. If you are diagnosed with diabetic retinopathy, we will recommend safe, effective solutions for your specific circumstances. Our recommendations will be tailored to the nature and severity of your disease.
Contact our retinal specialists today to learn more about treating diabetic retinopathy.



